Something that I’ve got a lot of mileage out of recently is bladder ultrasound.
This is a skill we learn as part of the FAST exam where the goal is to find free fluid that has accumulated in the pelvis due to trauma. Ultrasound of the bladder has a few other applications, which can be helpful in the right patient. Specifically, patients with complaints of urinary frequency or hesitancy, blood in their catheter bag, poor output from long term catheter, or pain after having a Foley catheter placed are cases where a quick look at the bladder can cut straight to the diagnosis and save you and the patient a lot of time and testing.
This is part 1 of series of posts about easily recognizable bladder pathology.
First of all, recall that just like during a FAST exam, the bladder should be imaged in two planes: short axis (probe marker to the patient’s right side) and long axis (probe marker to the patient’s head). For the sake of brevity, I didn’t include both images in all cases in the posts; but I’ve described each so it will be clear how the images were obtained.
Patient 1
A 74 year-old man who presented with pain and bleeding into the bag after a Foley catheter had been placed at an outside clinic for urinary retention. Our first concern was whether the catheter was in the bladder or obstructed.
Here we see the images on arrival. (All of these images are in long axis – probe marker towards the patient’s head.)

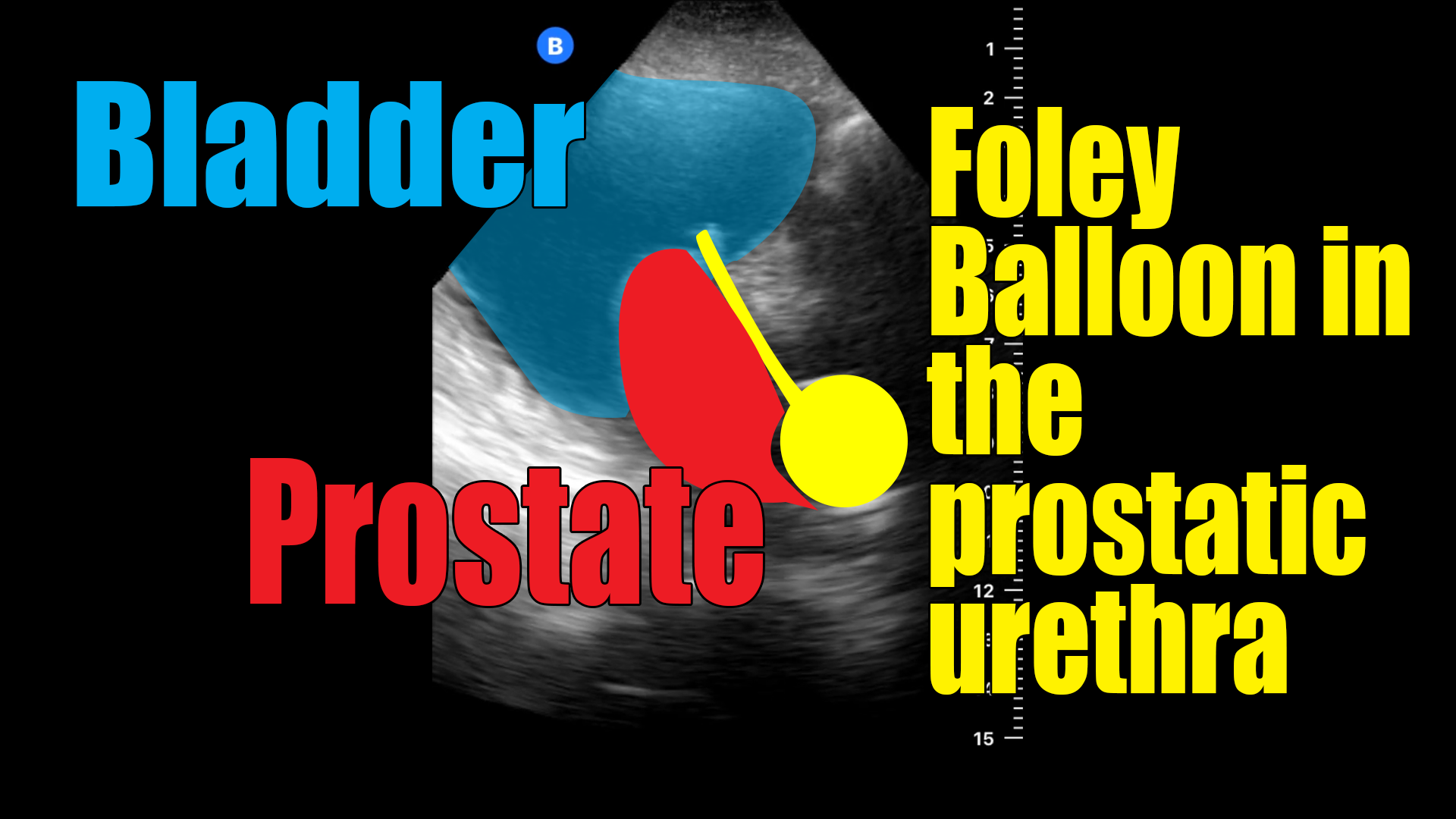
It’s clear from the images that the catheter was not fully inserted before the balloon was inflated. In this case, the tip appears to be within the bladder; so it is likely that there was urine obtained prior to the inflation, which usually is an indication that catheter is in the proper place.
Based on these images, the balloon was deflated and the catheter advanced. Once it was seen to be within the bladder, the balloon was reinflated and the following image was obtained.


If you find something like this, it’s worth a call to the urologist as the balloon can cause damage to the urethra. Although in this case the catheter was able to easily be advanced into the bladder – and was confirmed to be in the bladder with ultrasound prior to reinflating the balloon – there is risk of having created a tear in the urethra when the balloon was initially inflated. If that were the case, and if the reposition attempt had gone awry, the catheter could have been passed through the tear in the lumen into the pelvis. Although the tear is a problem, temporarily passing a catheter through the tear is not a catastrophic as it sounds (in my opinion). In my experience most on call urologist are okay with you attempting to reposition the catheter as long as it is not reinflated without confirmation that it’s in the bladder. That confirmation could be urine return or ultrasound. However, there could be some practice variation and subtlety here, so involving the specialist is never a bad idea.
When catheters aren’t flowing or are painful, there are several potential causes. Specifically, it could be malpositioned, as in this case, or it could be occluded. The ultrasound immediately differentiates between the two scenarios, which is very helpful because clearly the management is very different.