Forehead sparing, partial dual innervation, HSV, VZV, Ramsay Hunt, geniculate ganglion, zoster oticus, zoster opthalmicus, Hutchinson’s sign, nasociliary nerve, dendritic ulcers, topical steroids – it’s a lot of buzzwords. Let’s clarify. From the top…
Where is this coming from?
Two places:
This is the type of thing that confuses the students, residents, nurses, and attendings, so I wanted to make a list of all the buzz words and define them as a reference.
Specifically, though, we had a case with a Hutchinson’s sign (as defined in detail below) a few years ago. The resident on the case spoke with an ophthalmologist about their concern for the possibility of there being dendritic ulcers on the cornea. The eye doctor said something to effect of, “I’m happy to see them, but the thing you are worried about is caused by a different virus than what the patient has.”
Mic drop. Blog post. Here’s the scoop.
Bell’s Palsy
A clinical syndrome consisting of a motor weakness (droop) of both the lower and upper face. It is usually unilateral and is caused by interruption of cranial nerve VII, the facial nerve. (diagram) Common causes include herpes simplex virus, Lyme disease, tumors of the facial nerve, middle ear pathology, and varicella zoster virus.
Forehead Sparing
When evaluating a patient with a motor weakness of the face, the pivotal part of the diagnosis is differentiating whether the problem is coming from the motor cortex (a stroke) or from an insult to the facial nerve itself. Fortunately, the two entities can be neatly separated by how the muscles of the forehead are affected. Lesions of the facial nerve involve the entire face: the patient will have weakness or paralysis of both the lower face (manifested by the inability to smile on the affected side) and the forehead (inability to raise the affected eyebrow). If the problem is coming from the motor cortex, on the other hand, the weakness “spares” the muscles that move the forehead. There will be weakness of the muscles of the lower face, but the brow will raise normally on the affected side. (diagram)
It’s important to realize that the weakness of the forehead may not be a complete paralysis. Any weakness points to a peripheral cause.
Partial dual innervation
The facial nerve has both motor and sensory neurons. The cell bodies of the motor neurons are located in the facial nerve nucleus, which is in the pons. The facial nerve nucleus has two divisions: dorsal and ventral. Both divisions get input from upper motor neurons originating in the motor cortex. The dorsal division controls the muscles of the forehead and gets input from both (right and left) motor cortices. The ventral division of the facial nerve nucleus controls the muscles of the lower face. Unlike the dorsal division, the ventral division only gets upper motor neuron input from the ipsilateral motor cortex.
This is why people with cerebrovascular accidents involving the part of the motor cortex that controls the face can still raise their eyebrow on the affected side – the dorsal division has input from the unaffected (contralateral) motor cortex, which remains functional in the setting of a stroke. The lower part of the face, however, is weak in the setting of a stroke, because there is no backup control from the opposite motor cortex. (diagram)
Herpes Simplex Virus (HSV) vs Varicella Zoster Virus (VZV)
Both of these viruses are in the herpesvirus family. Both have latent phases and can reactivate to cause disease. Both cause vesicular rashes. Both lie dormant in sensory (not motor) neurons. When VZV reactivates, it causes a rash along the dermatome of the affected sensory nerve, whereas HSV usually reactivates in clusters along the affected sensory nerve’s zone of dermal innervation. VZV causes the clinical syndromes known as chicken pox and shingles. HSV can cause several clinical syndromes including orolabial and genital herpes, encephalitis, and keratitis.
Ramsay Hunt Syndrome
Bell’s palsy is a clinical syndrome with more than one cause. In some cases, the cause can be identified (otitis media, Lyme disease, tumors of the facial nerve), but most of the time it is idiopathic and thought to be caused by herpes simplex virus. Occasionally, however, it is caused by varicella zoster virus reactivating in the sensory (not motor) ganglion of the facial nerve: the geniculate ganglion.
Recall that the rash associated with zoster appears in the distribution of skin whose sensory innervation is supplied by the nerve the virus was dormant in. Below the face, that separates neatly into dermatomes corresponding to spinal nerves. Since the facial nerve only provides skin innervation to the ear canal, its “dermatome” is limited to that location. Indeed you would see a vesicular rash in the external auditory canal in the setting of zoster originating from the geniculate (sensory) ganglion of the facial nerve. The Bell’s palsy (motor weakness) associated with Ramsay Hunt syndrome is due to the proximity of the motor fibers passing through/near the inflamed geniculate ganglion on their way to the periphery.
Finding this entity is one reason* it is important to look in the ear of anyone with Bell’s palsy. Treatment for nonspecific Bell’s palsy generally consists of oral steroids with or without antiviral medications. Recommendations change periodically as to whether or not the antivirals are recommended in all cases. In the case of Ramsay Hunt syndrome, however, you would certainly use antivirals (particularly if they can be started early) as this entity is not “likely” to be caused by a virus as is the case with idiopathic Bell’s palsy, but “certainly” caused by a virus.
*Another reason to look in the ear of anyone with Bell’s palsy, is that a Bell’s palsy can be caused by an otitis media/middle ear effusion. You’d hate to assume something is idiopathic when in fact there is a treatable cause if you’d just taken the time to look.
Geniculate Ganglion
The facial nerve has both motor and sensory functions. Cell bodies of the motor neurons are located in the pons at the facial nerve nucleus. Cell bodies of the sensory nerves are located in the periphery in the geniculate ganglion. This is where VZV reactivates from to cause Ramsay Hunt syndrome.
Zoster Oticus
This is another name for Ramsay Hunt syndrome. Varicella zoster virus reactivation from the geniculate ganglion causing vesicles in the ear canal and usually a Bell’s palsy. This is a type of zoster involving the face, but this does not come from one of the three branches of the trigeminal nerve. This one is from the facial nerve.
Zoster Ophthalmicus
Contrary to the motor innervation to the muscles of the face, which is supplied by the facial nerve (cranial nerve VII), the trigeminal nerve (cranial nerve V) provides the sensory innervation of the face. Three large branches cover the face and merge in the trigeminal ganglion, where viruses like VZV can lie dormant. The three branches are the opthalmic (V1), maxillary (V2), and mandibular (V3). Zoster ophthalmicus is reactivation of VZV in the V1 branch of the trigeminal nerve and would present clinically as a vesicular rash on the forehead.
Hutchinson’s Sign
In the setting of Zoster opthalmicus, the presence of vesicles on the tip or side of the nose is called Hutchinson’s sign. Its clinical significance is that its presence means there is likely to be corneal involvement, and we should be thorough to look for it.
The tip of the nose is innervated by branches of the anterior ethmoidal nerve, which are branches of the nasociliary nerve. The cornea is innervated by the long ciliary nerves, which are also branches of the nasociliary nerve.
Hutchinson’s sign means the nasociliary nerve is involved, therefore is a strong predictor that other branches of the nasociliary nerve might be involved as well (i.e., the long ciliary nerve and therefore the cornea).
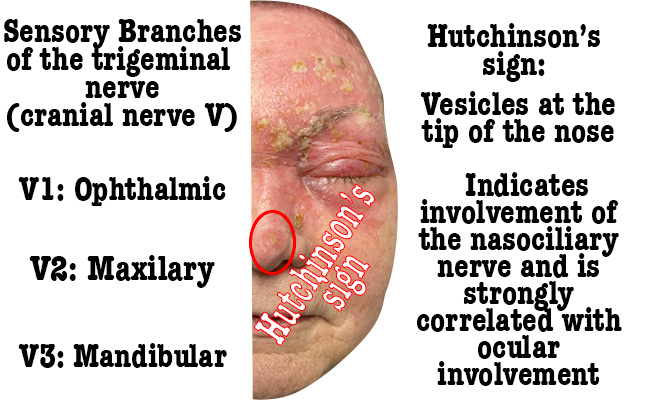

Nasociliary nerve
A branch of the V1 (opthalmic) branch of the trigeminal herve, the nasociliary nerve provides branches to the cornea and the tip of the nose (among other things). Vesicles at the tip of the nose (Hutchinson’s sign) indicate involvement of the nasociliary branch of V1, and therefore the possibility that the cornea could be involved.
Dendritic ulcers on the cornea
This is a red herring in the discussion of zoster, because it is not caused by varicella zoster virus. Rather, “dendritic ulcers” are caused by herpes simplex virus. The “ocular involvement” we worry about in the presence of Hutchinson’s sign is in the setting of varicella zoster virus, not herpes simplex virus.
HSV keratitis would likely present in isolation (a painful red eye) rather than in the setting of a vesicular rash in a dermatomal distriubtion as is the case in zoster ophthalmicus/Hutchinson’s sign.
The diagnostic and treatment differences between HSV keratitis and VZV keratitis are subtle. Both would need to be evaluated by an ophthalmologist.
Topical Steroids
We hold this truth to be self evident: do not put topical steroids in the eye of someone with herpes keratitis, i.e. a dendritic ulcer, because it will make things worse. (There is actually some subtlety to this decision based on the layer of the corenea affected, etc – things I wouldn’t have a way to know in the moment.)
Because of the chance of this, I think most of us (EM providers) don’t put topical steroids in anyone’s eye unless an eye doctor tells us to do so. Unlike HSV keratitis, VZV keratitis produces a “pseudo-dendritic” ulcer, which affects different layers of the corena than the “dendritic” lesion of HSV keratitis classically affects. There “may” be a role for topical steroids in VZV keratitis, but again I’d let the eye doctor make that decision.

