After years of searching, I finally came across a few cases of retinal detachment. They are usually simple, but one similar diagnosis shows up when we learn about these things. There is an easy way to tell them apart, but you have to know what you are doing. Let’s have a look.
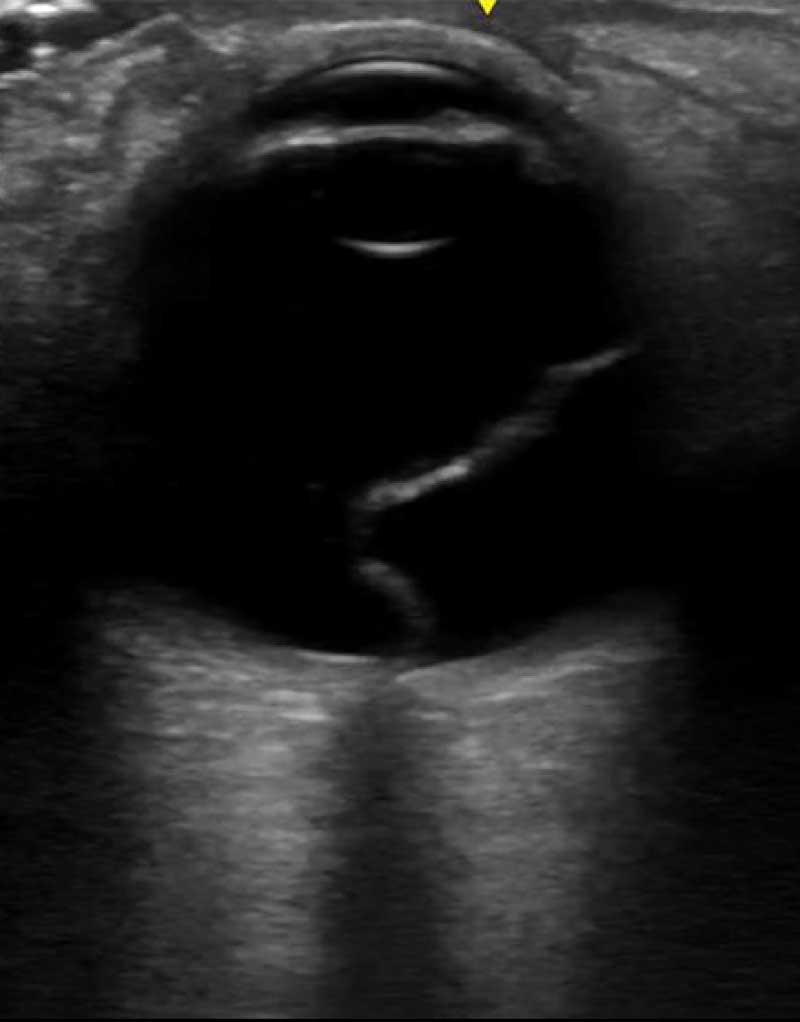
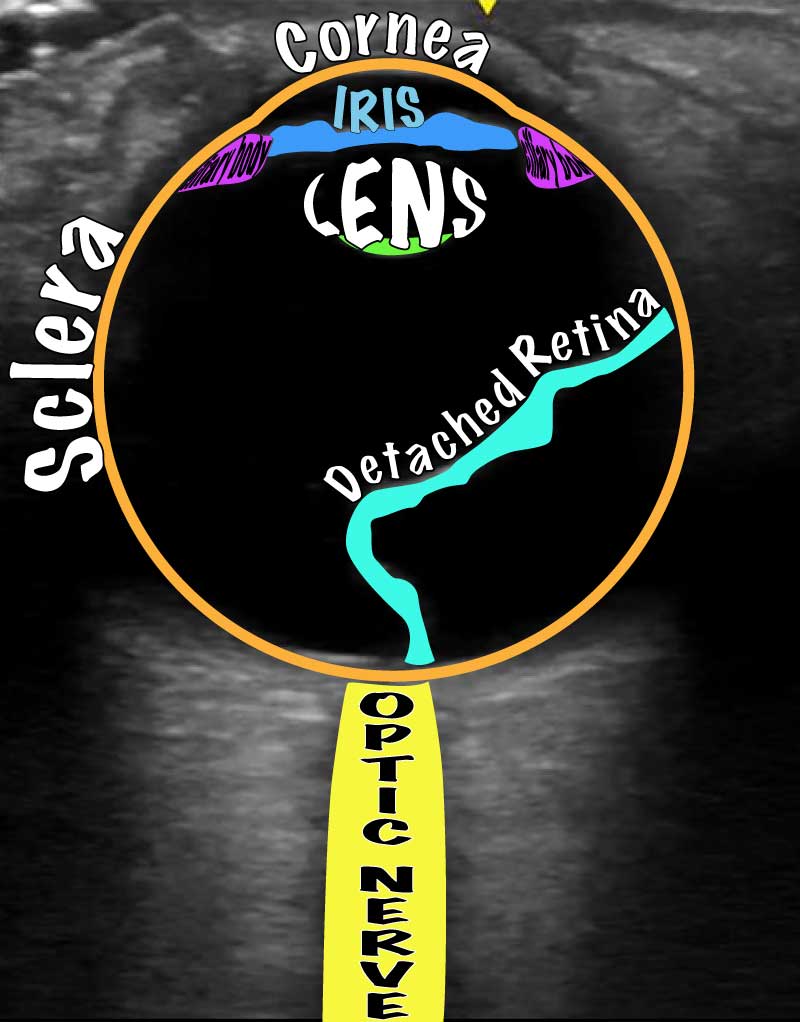
Eyeballs are superficial, fluid filled structures and therefore low-hanging fruit for point of care ultrasound. Retinal detachments are generally easy to see and look like a serpentine structure in the back of the eye.
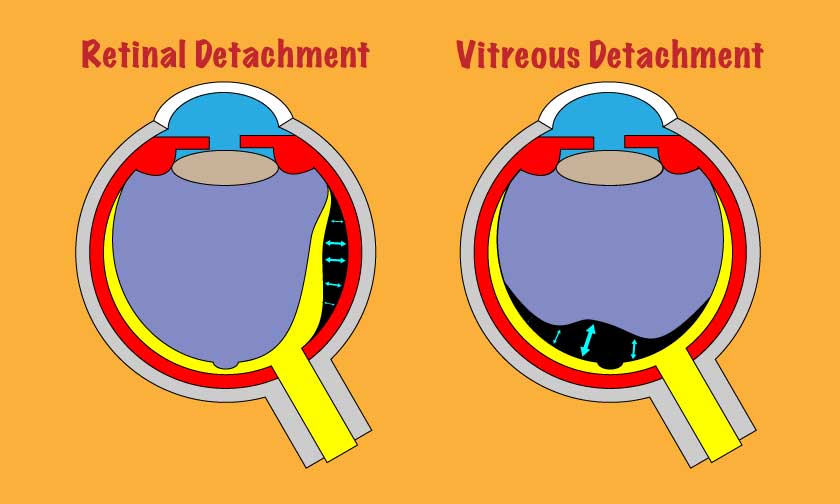
Unfortunately, there is one red herring diagnosis that looks similar: a vitreous detachment. On-line resources as well as hands-on seminars (understandably) feel compelled to discuss both. While I understand the need to be thorough, I worry this leads to confusion among learners. In trying to teach residents about anything – not just ultrasound – I live in fear of them wielding their new tools and knowledge before they have the full depth of understanding that they think that they have (the dreaded “unconscious incompetence”). To that end, let’s spend a few minutes and see what makes a retinal detachment distinct from a vitreous detachment.
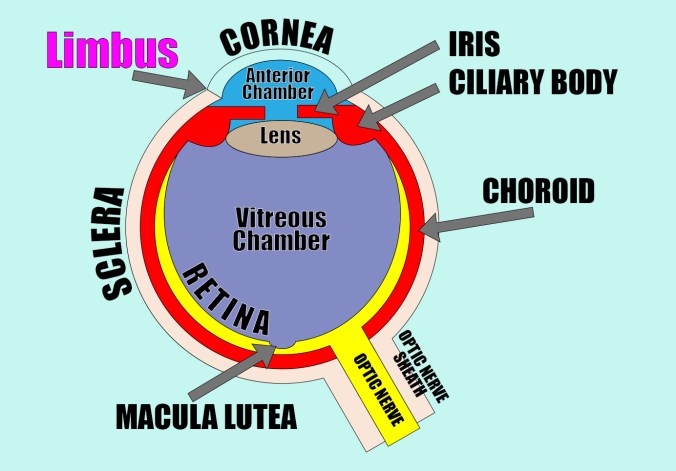
Anatomy
The diagram makes it clear that several of the named structures are continuous with/extensions of one another. Understanding that helps you appreciate where detachments can occur.
Specifically, the optic nerve sheath is continuous with the sclera and cornea; the choroid is continuous with the ciliary body and iris (the three together comprise the “uvea”); and the retina is an extension of the optic nerve.
Ultrasonographic anatomy of a retinal detachment
Importance of visualizing the optic nerve
The retina is not usually visible. When it detaches, however, it becomes very conspicuous. The crucial thing to remember is that since it is an extension of the optic nerve, the two structures will always be attached. Detached retinas don’t float freely; they are tethered to the optic nerve. Vitreous detachments, on the other hand, are not anchored to the optic nerve. They do float freely.
With that in mind, it is clear why to differentiate the two on ultrasound, you MUST include the optic nerve on the scan. Also keep in mind that the ultrasound is a two dimensional slice of a three dimensional structure. If you do not visualize all the way through it, you will be fooled at times. It is essential that you sweep through the globe in two different planes and include the optic nerve.
Examples of the retina tethering to the optic nerve


How could I mess this up?
A related, but slightly tangential case
Final Thoughts
The subtlety on the ultrasound is fun, and it is good to know everything. However, don’t forget that retinal detachments present acutely with vision loss. Vitreous detachments classically do not. The vitreous does not have a vision essential function and detaches in many people’s eyes as they age without much consequence.
If you have a patient in front of you with acute vision loss and something like this on their ultrasound, you should assume it is a retinal detachment. Be thorough. Be informed. But, don’t over think it. If the history is consistent with retinal detachment, go with that until a specialist proves you wrong.
It is worth noticing that I don’t have a video of a vitreous detachment to show you. That’s because it is not an acute problem. People do not come to the emergency department because of it. That’s why at the beginning of the post I said that knowing about them makes retinal detachments seem more complicated than they are. If you have someone with acute unilateral vision loss and something concerning in the eye on ultrasound, you should assume it is the retina.
Scan happy, my friends.

Pingback: How Gain Settings Affect Vitreous Imaging | Searcy EM