Not all “Paced” EKGs are the same. Let’s look at some of the differences among them.
Three examples of EKG tracings in people who are being paced
There are some differences. They are straight forward once you have a grasp on it, but I frequently see learners that have not yet had their light bulb moment. Can you sort out the subtleties among these?

Where do we start?
Start with the facts that P waves represent atrial depolarization, and QRS complexes represent ventricular depolarization. Then remember that most pacemakers have an atrial lead and a ventricular lead. (Other configurations exist but are less common). These leads can both sense underlying electrical activity and can generate an electrical impulse, which will depolarize any nearby cardiac myocytes. That depolarization is then propagated from myocyte to myocyte resulting in ventricular contraction. The deflection caused by the pacemaker impulse seen on the EKG is often referred to as a “spike.” The device’s settings as to which chambers are sensed and/or paced are selected by the cardiologist based on the patient’s individual physiology.
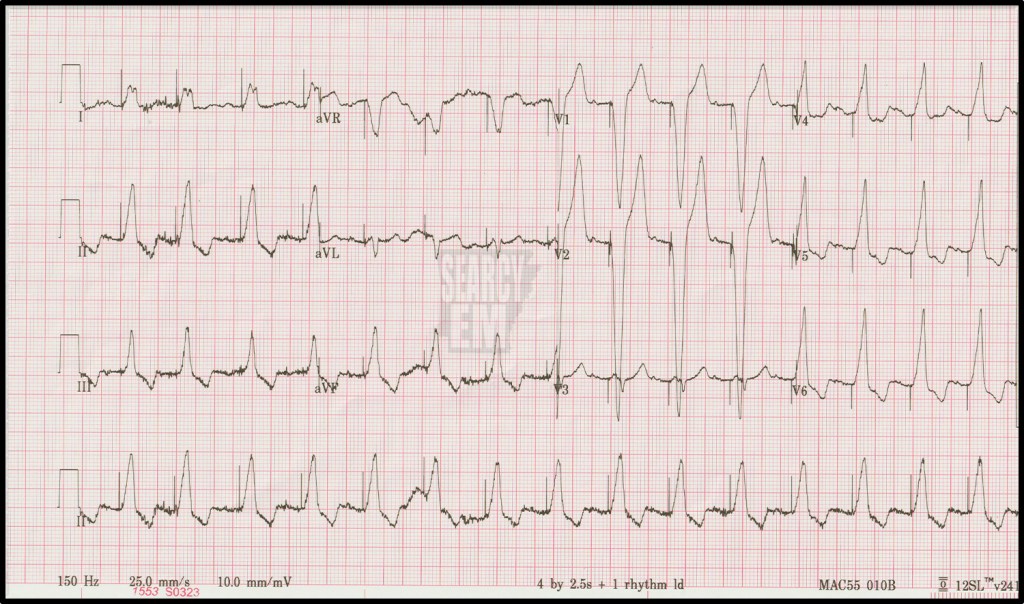
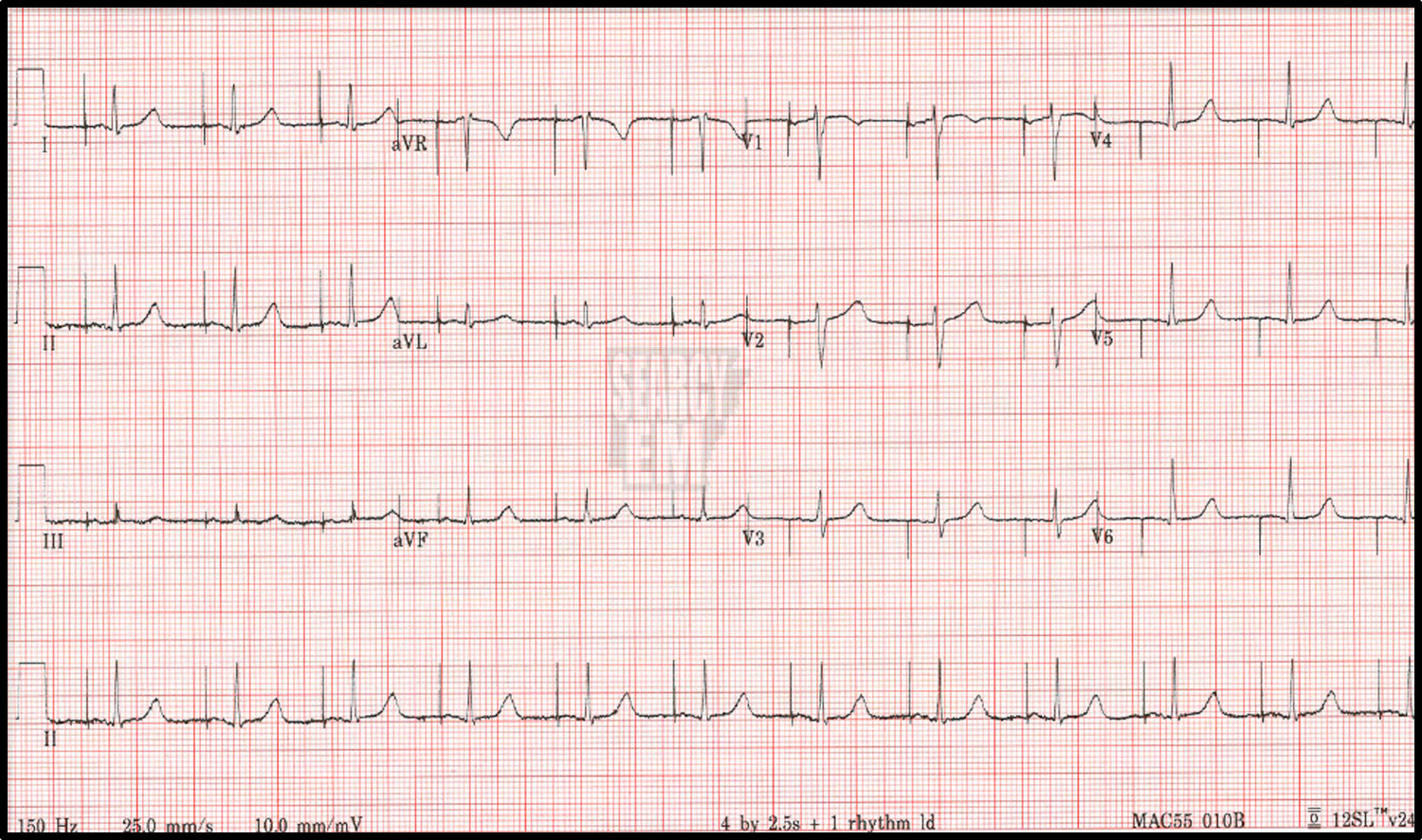
If the pacer spikes fall before the P waves, the atria are being paced.
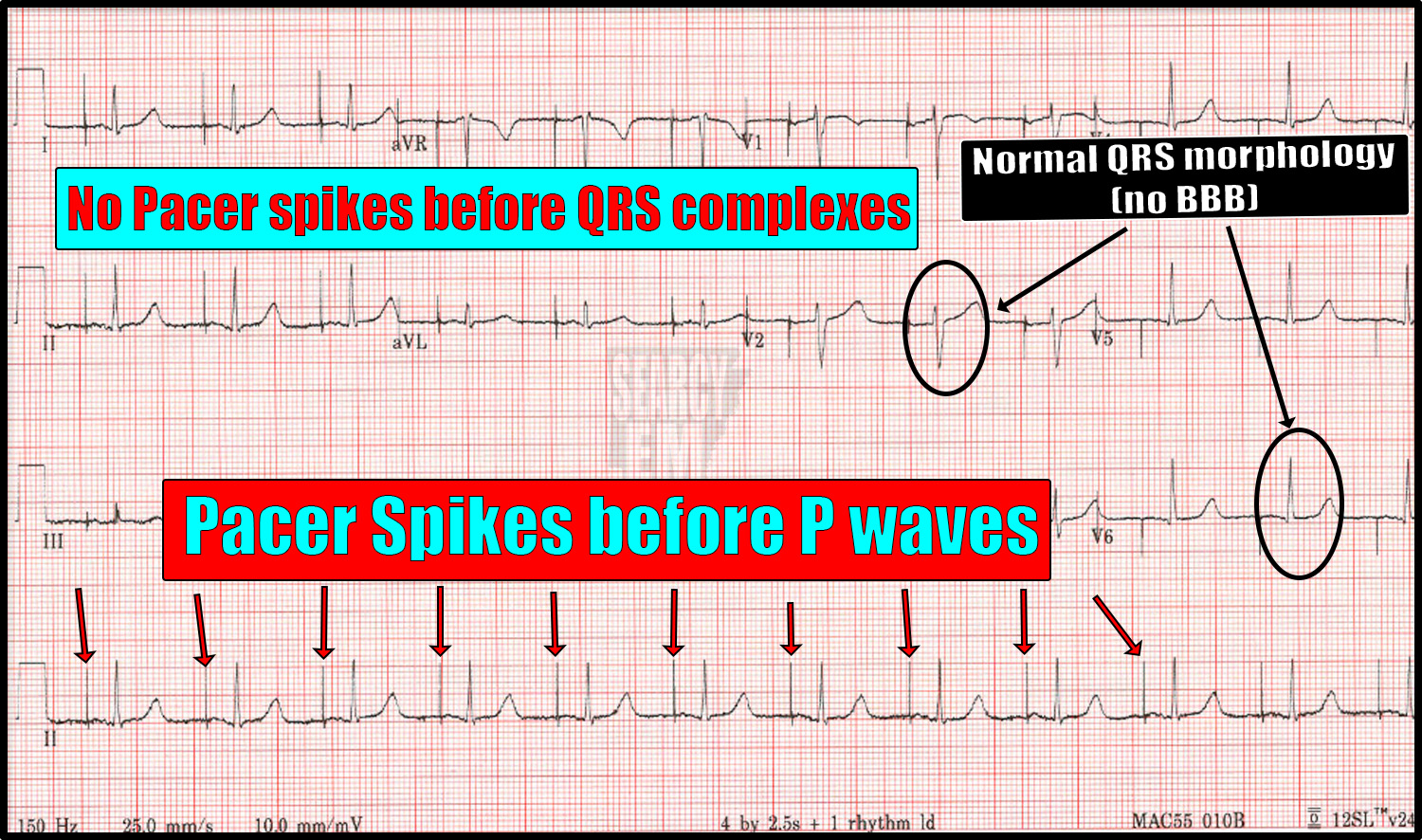
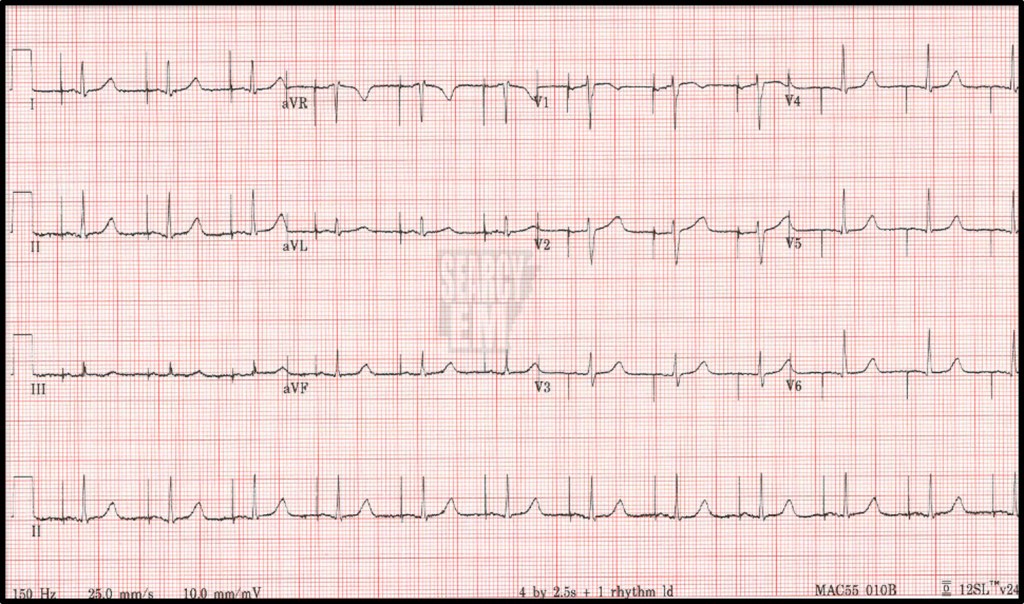
If a pacer spikes fall before the QRS complexes, the ventricles are being paced.

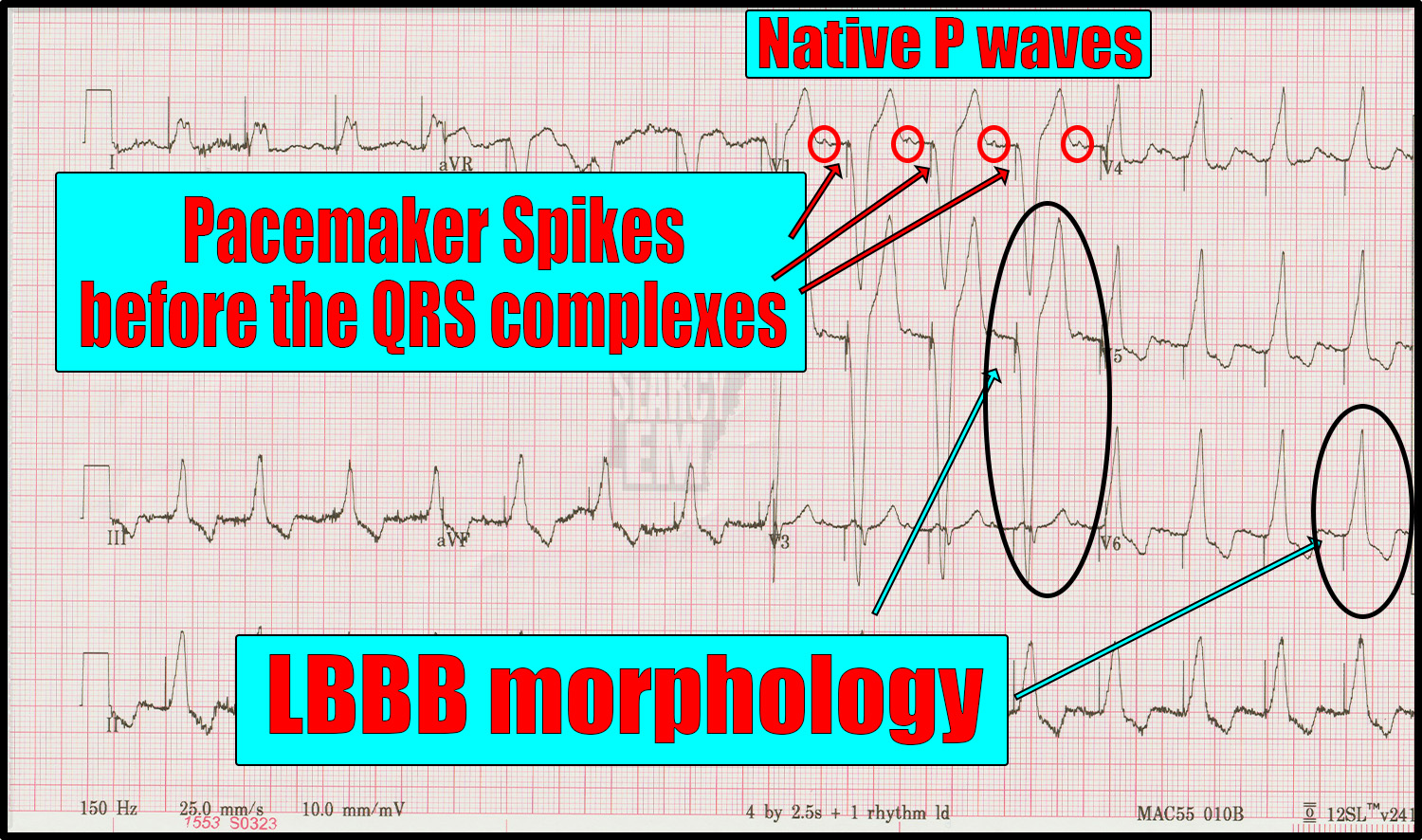
If we see native P waves (as in the example above) followed by a pacer spike before the QRS complex, the atria is being sensed and the the pacemaker responds to that atrial depolarization by stimulating a ventricular contraction: atrial sensed, ventricular paced. This type of rhythm would still show the usual variation in heart rate that we see in people throughout the day because the SA node is dictating that rate. On the other hand, if someone were in a ventricular paced rhythm with underlying atrial fibrillation, there would be no point in “sensing” for P waves and reacting to them. Those patients have a “ventricular paced” rhythm “without atrial sensing.” Their rate would fall to the default setting and would not change throughout the day.
If the pacer spikes occur before both the P waves and the QRS complexes, then both the atria and the ventricles are being paced independently.
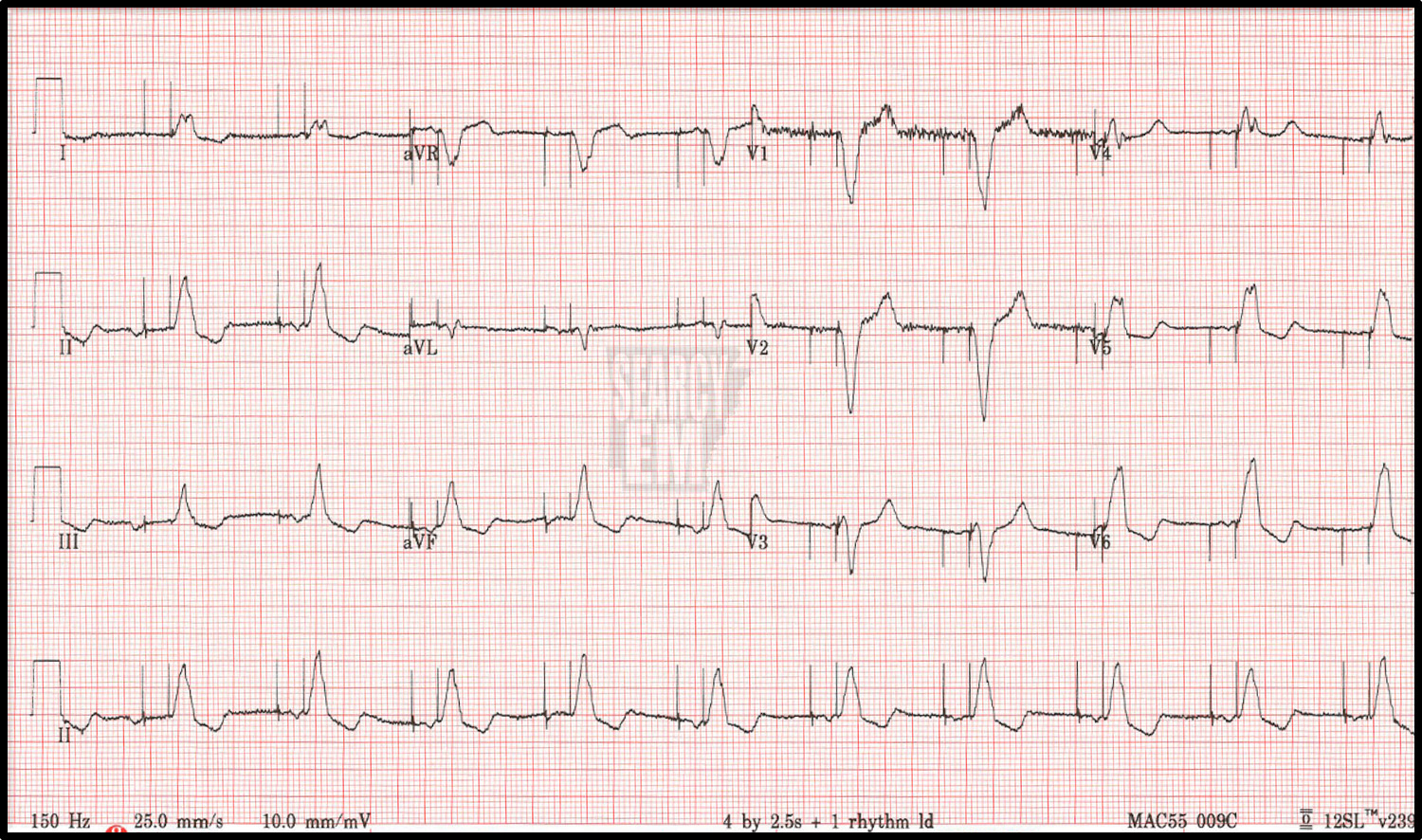
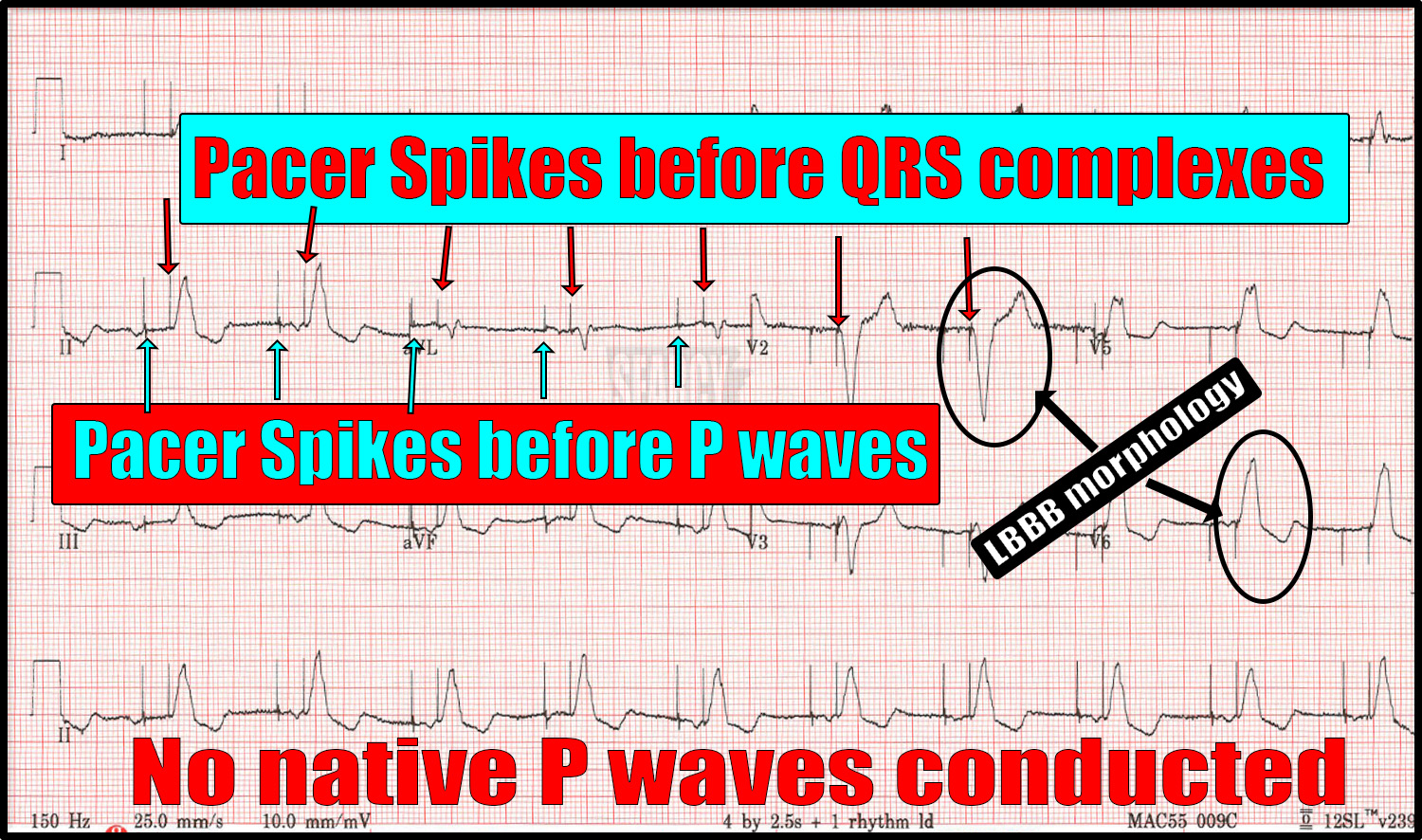
This setting also dictates the rate, but pacing both the atria and the ventricles allows for an “atrial kick.”
[The details of exactly which patient needs which setting is beyond the scope of this review.]
Differences in depolarization
Notice that if only the atria are being paced (the first example above), the depolarization still spreads through the AV node, into the bundle of His, and through the Purkinje fibers in the usual fashion. That means that unless there is an underlying bundle branch block, the QRS complex will be narrow. Nothing the pacemaker is doing is affecting the electrical propagation – it just initiates it.
On the other hand, if the ventricle is being paced (second and third examples above), the depolarization does not travel down the conducting system. The impulse is spread from cell to cell in the same manner as we see in a bundle branch block, which results in a wide QRS complex. Indeed, ventricular paced rhythms classically look like a left bundle branch block.
Why does this matter to me as the ED provider?
The most tangible benefit to understanding these things comes up when evaluating for acute ischemia.
If the pacemaker is only pacing the atria, the standard conduction pathways are in use and ST segment changes are fair game. The usual diagnostic criteria for STEMI can be applied.
On the other hand, the issue is less clear when the ventricles are being paced. We have criteria (several iterations, in fact) that we can use to identify acute ischemia in the setting of a left bundle branch block (1,2,3). There is evidence that these criteria can be applied to the LBBB seen in ventricular paced rhythms as well (4). And although there is not complete acceptance of this line of thought, I would certainly take notice if a patient with a ventricular paced rhythm and chest pain concerning for ACS had an EKG that met Smith-modified Sgarbossa criteria.
Summary
Not all “paced” EKGs are the same. Some leave the door open to the usual diagnostic modalities in terms of ischemia while others require a bit more thought. However, don’t throw out the baby with the bath water when you see a paced rhythm. There can still be relevant information gleaned even when there are spikes on the paper.
References
- Sgarbossa EB. Value of the ECG in suspected acute myocardial infarction with left bundle branch block. J Electrocardiol. 2000;33 Suppl:87-92. doi: 10.1054/jelc.2000.20324. PMID: 11265742.
- Smith SW, Dodd KW, Henry TD, Dvorak DM, Pearce LA. Diagnosis of ST-elevation myocardial infarction in the presence of left bundle branch block with the ST-elevation to S-wave ratio in a modified Sgarbossa rule. Ann Emerg Med. 2012 Dec;60(6):766-76. doi: 10.1016/j.annemergmed.2012.07.119. Epub 2012 Aug 31. Erratum in: Ann Emerg Med. 2013 Oct;62(4):302. PMID: 22939607.
- Di Marco A, Rodriguez M, Cinca J, Bayes-Genis A, Ortiz-Perez JT, Ariza-Solé A, Sanchez-Salado JC, Sionis A, Rodriguez J, Toledano B, Codina P, Solé-González E, Masotti M, Gómez-Hospital JA, Cequier Á, Anguera I. New Electrocardiographic Algorithm for the Diagnosis of Acute Myocardial Infarction in Patients With Left Bundle Branch Block. J Am Heart Assoc. 2020 Jul 21;9(14):e015573. doi: 10.1161/JAHA.119.015573. Epub 2020 Jul 4. Erratum in: J Am Heart Assoc. 2020 Nov 17;9(22):e014618. doi: 10.1161/JAHA.119.014618. PMID: 32627643; PMCID: PMC7660719.
- Dodd KW, Zvosec DL, Hart MA, Glass G 3rd, Bannister LE, Body RM, Boggust BA, Brady WJ, Chang AM, Cullen L, Gómez-Vicente R, Huis In ‘t Veld MA, Karim RM, Meyers HP 3rd, Miranda DF, Mitchell GJ, Reynard C, Rice C, Salverda BJ, Stellpflug SJ, Tolia VM, Walsh BM, White JL, Smith SW; PERFECT study investigators (the complete list of PERFECT study investigators is provided in Appendix E1, available at http://www.annemergmed.com). Electrocardiographic Diagnosis of Acute Coronary Occlusion Myocardial Infarction in Ventricular Paced Rhythm Using the Modified Sgarbossa Criteria. Ann Emerg Med. 2021 Oct;78(4):517-529. doi: 10.1016/j.annemergmed.2021.03.036. Epub 2021 Jun 23. PMID: 34172301.
