What’s wrong in this picture?
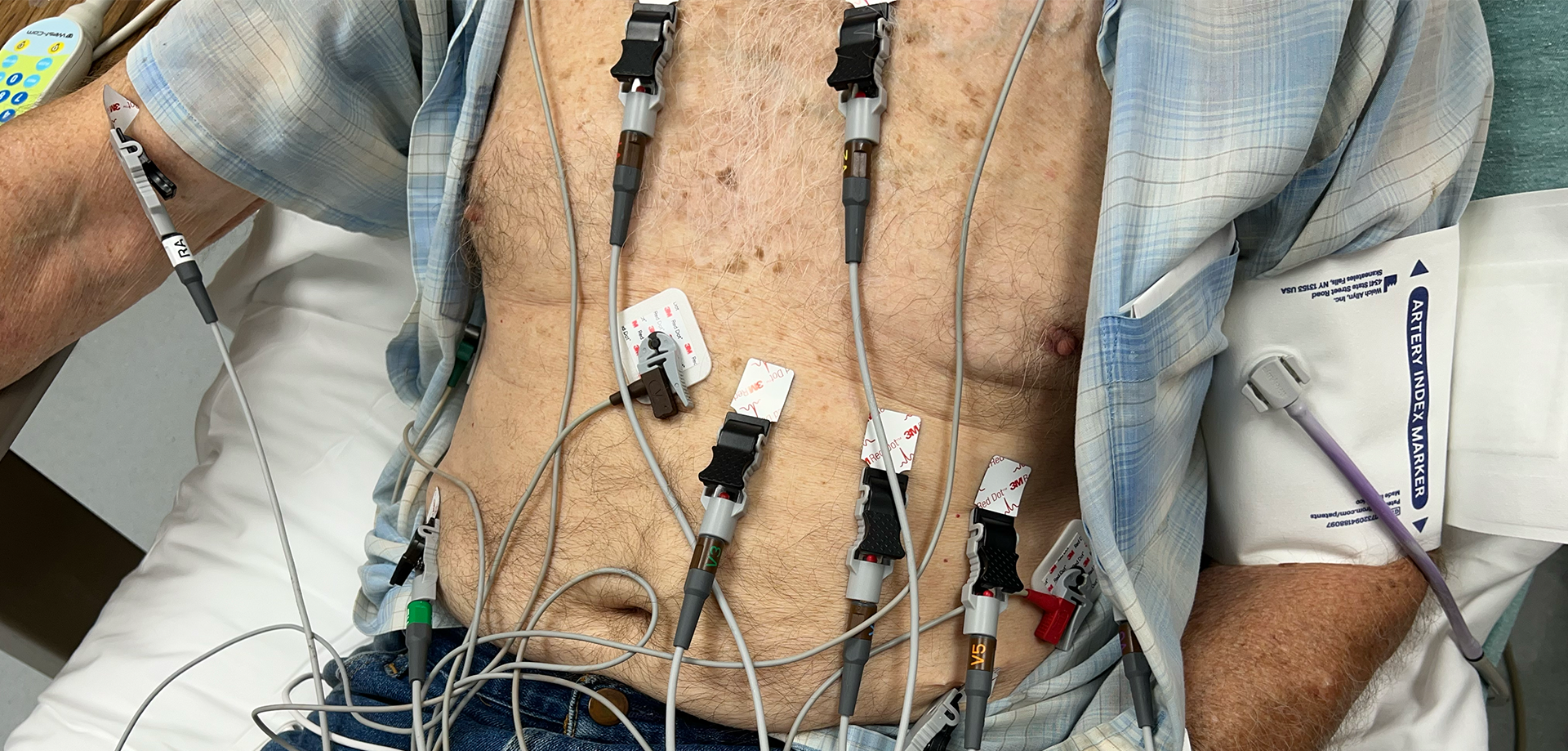
Notice the position of the chest leads.

V3 is the anatomic right of V2. That is no good.
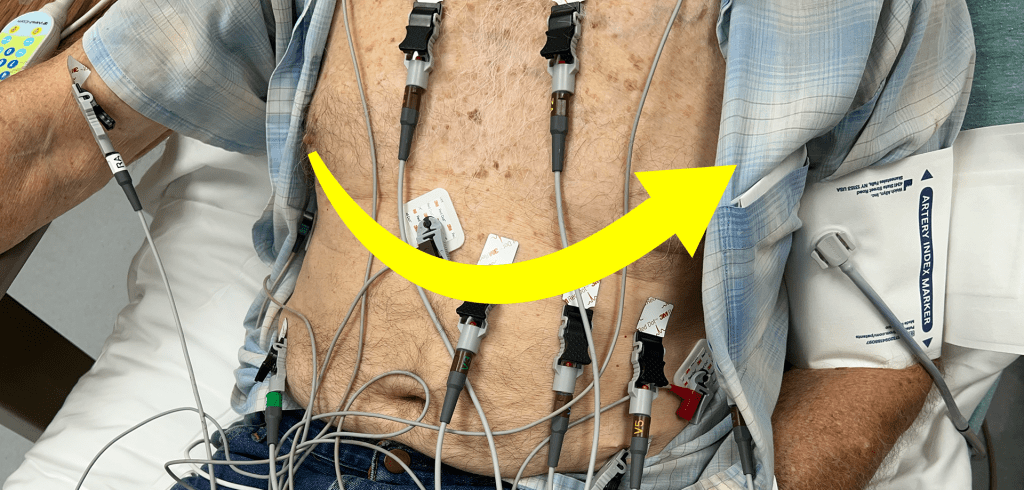
The position of the chest leads should be anatomic right to left. No lead should be to the anatomic right of the lead prior to it. This configuration allows us to see the axis in the axial plane.
We may not spend much time on that concept – the axis in the axial plane. Usually when we think of the “axis” of an electrocardiogram, we are thinking of the coronal plane using the limb leads:

However, if you take the time to consider “R wave progression” you are doing the same thing with the chest leads and axial plane that a traditional “axis” is measuring in the limb leads and the coronal plane.

What do the guidelines say?
In a position statement in published in 2007, the AHA/ACC/HRS published “Recommendations for the Standardization and Interpretation of the Electrocardiogram, Part 1: The Electrocardiogram and Its Technology” the lead positions are defined as follows:
“V1, fourth intercostal space at the right sternal border; V2, fourth intercostal space at the left sternal border; V3, midway between V2 and V4; V4, fifth intercostal space in the midclavicular line; V5, in the horizontal plane of V4 at the anterior axillary line, or if the anterior axillary line is ambiguous, midway between V4 and V6; and V6, in the horizontal plane of V4 at the midaxillary line.”
This definition specifically states that V3 should be “midway between V2 and V4.” Plain as day. It actually brings up another problem in the above example. This paper says leads V1 and V2 should be in the 4th intercostal space, and Lead V4 should be in the 5th intercostal space: that’s only one rib space apart! In our picture above, leads V1 and V2 are probably two rib spaces too high with the others a rib space too low. The authors specifically state in the body of the article that superior misplacement of leads V1 and V2 is common and lead to low R wave amplitudes by 0.1 mV per rib space and can cause a rSr’ pattern with t wave inversions.
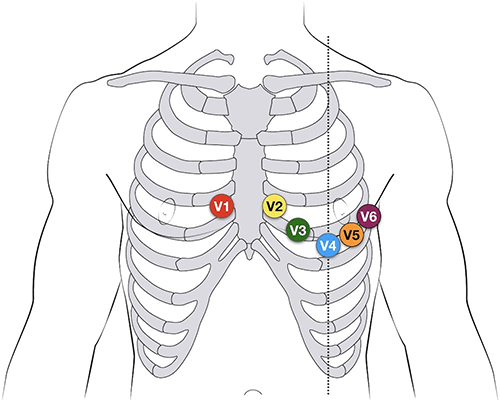
The above image was borrowed from Life in the Fast Lane and shows positioning of the electrodes in positions close to those described in the paper above. I say “close” because in this diagram, V4, V5, and V6 actually follow the 5th intercostal space rather than the “horizontal plane of V4”. The AHA/ACC/HRS paper quoted above actually acknowledges that there is “some residual disagreement” about which is the best place for those three leads. It describes the positioning in the image above (all three leads in the 5th intercostal space) as “an early recommendation” and implies that it is outdated. Now, that it some high level minutia – even to me.
Where are the dead bodies?
Admittedly, there probably are not many people where this lead positioning would result in missing a critical diagnosis in the ED. We as EM providers don’t make a lot of life and death decisions based on the R wave progression. I suppose if you were looking for ST elevation in contiguous leads, having the leads in this position may put V2 “between” V3 and V4 thus making elevation in those leads appear to be non-contiguous. But even then, I suspect we could work through that in real time.
One real issue is that of reproducibility. We often do serial electrocardiograms. If we use correct lead placement on one and haphazard placement on the next, it could give the illusion of dynamic changes.
Another is the effect of lead positioning on measurements. Left ventricular hypertrophy, for example, is a judgment based on amplitude. Lead positioning could certainly affect that.
At some level, however, it’s the principal of the thing. If we are going to do tests on people, we should do them correctly. We owe them that much. If we are sloppy on this sort thing, what else with more tangible consequences are we letting get by without proper scrutiny?
References
Kligfield P, Gettes LS, Bailey JJ, Childers R, Deal BJ, Hancock EW, van Herpen G, Kors JA, Macfarlane P, Mirvis DM, Pahlm O, Rautaharju P, Wagner GS; American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; American College of Cardiology Foundation; Heart Rhythm Society. Recommendations for the standardization and interpretation of the electrocardiogram. Part I: The electrocardiogram and its technology. A scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Heart Rhythm. 2007 Mar;4(3):394-412. doi: 10.1016/j.hrthm.2007.01.027. Epub 2007 Feb 1. PMID: 17341413.